Translate this page into:
Successful in vitro fertilization pregnancy in a case of unicornuate uterus with diminished ovarian reserve: A case report
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The occurrence of Mullerian anomalies with concomitant gonadal abnormalities is very rare. Very limited number of case reports are published in the literature, and the exact incidence is not known. In this report, we present a case of unicornuate uterus with non-communicating rudimentary horn along with absence of adnexa on one side and smaller ovary on other side, leading to diminished ovarian reserve. The patient conceived with in vitro fertilization (IVF) with oocyte donation and delivered a healthy child at 38th week of gestation. Establishing an accurate diagnosis and management by IVF followed by adequate supervision of resulting pregnancy may lead to successful obstetric outcome in women with unicornuate uterus with diminished ovarian reserve.
Keywords
Diminished ovarian reserve
pregnancy
rudimentary horn
unicornuate uterus
INTRODUCTION
The uterus develops from the fusion of paired paramesonephric ducts during the 10th week of gestation. There are a series of steps in this process starting from elongation, canalization, fusion, and finally resorption of midline tissue by the 20th week of gestation resulting in the formation of uterus, cervix, and fallopian tubes. Any aberration in this development process leads to different types of mullerian anomalies which are classified according to American fertility society (AFS) classification into seven types.[1] Unicornuate uterus results from a complete or partial failure of development of one of the paramesonephric duct. According to AFS classification, it falls under type II and is further subclassified into four variants:
With rudimentary horn.
With cavity:
Communicating;
Noncommunicating.
Without cavity.
Without rudimentary horn.
The reported incidence of unicornuate uterus is 1:4020 women in general population but is significantly higher in infertile women.[2] Ovaries which develop from urogenital ridge are generally present on the affected side but the position may be higher in the abdomen. There are few case reports in literature where ovarian abnormalities are associated with unicornuate uterus such as ectopic ovaries, unilateral ovarian agenesis or hypoplasia.[3,4] Breborowicz et al. reported two cases of congenital unilateral ovarian hypoplasia but without any mullerian anomaly.[5] To the best of our knowledge, this is the first case where unicornuate uterus is associated with unilateral ovarian hypoplasia leading to diminished ovarian reserve.
CASE HISTORY
A 25-year-old woman presented as a case of primary infertility of 2 years. She had a history of regular menstrual cycle of 25–26 days with flow duration of 3–4 days. There was no coital difficulty. She had congenital strabismus in both eyes, for which a corrective surgery was performed in childhood. There was a history of laparoscopic surgery for right adnexal mass at the age of 16 years, for which no record was available. Her father was diabetic. Her general, systemic, and pelvic examination was normal. Laboratory investigations revealed normal blood sugar, thyroid stimulating hormone (TSH) and prolactin levels, basal serum follicle stimulating hormone (FSH) 8.35 mIU/mL, luteinizing hormone (LH) 2.61 mIU/mL, estradiol 36.23 pg/mL, progesterone 0.41 ng/mL, and serum antimullerian hormone (AMH) level of 0.1 ng/mL. Semen parameters of husband were within normal limits as per World Health Organization (WHO) standards 2010.[6] On transvaginal songraphy, uterus was 73 mm × 28 mm × 41 mm with endometrial lining of 6.4 mm, left ovary was smaller in size (25 mm × 20 mm × 21 mm) with volume of 5.47 cc and antral follicle count (AFC) of 3–5, but the right ovary could not be visualized [Figure 1]. Hysterosalpingogram revealed unicornuate uterus, tubal block, and surgical staplers on right side [Figure 2]. The patient was then scheduled for diagnostic laparoscopy and hysteroscopy. The operative findings were as follows.

- Ultrasonographic image showing uterus and left ovary with 3–5 antral follicles
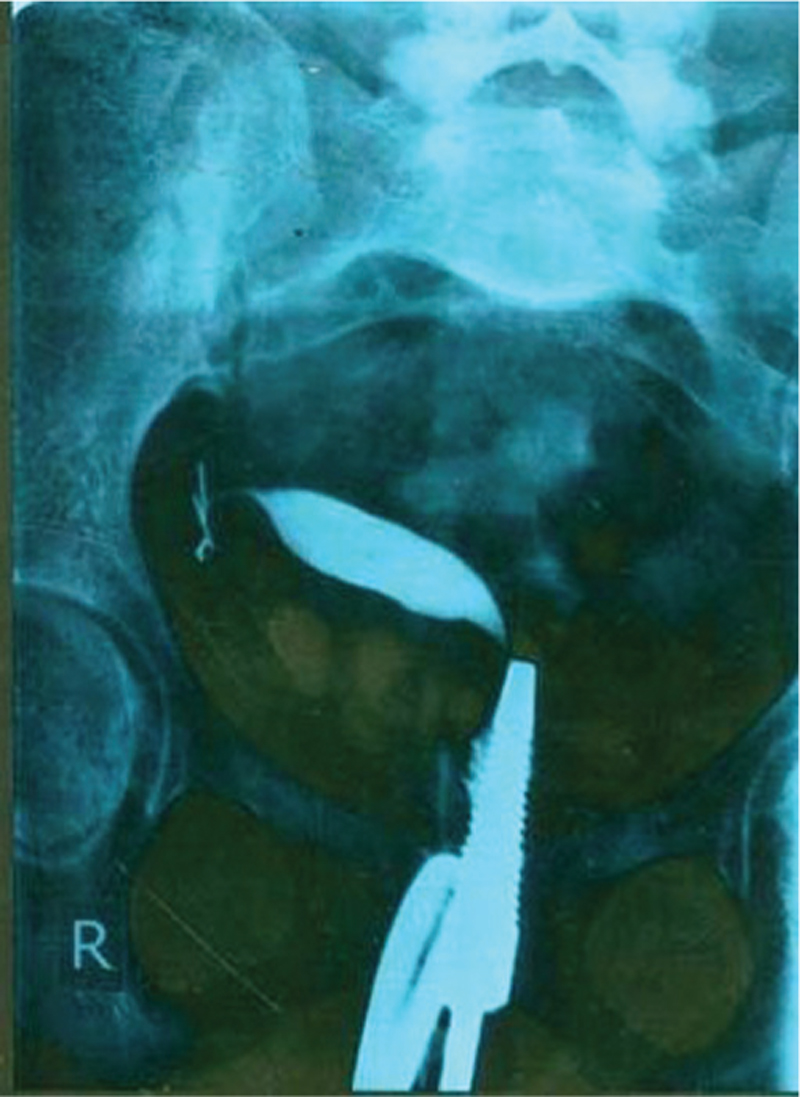
- Hysterosalpingography image shows right side deviated unicornuate uterus with surgical staplers on right side and tubal block
Hysteroscopy: Uterocervical length (UCL) 3 in., anteverted, normal endocervical canal, cavity was unicornuate with right horn as only the right ostium was seen, endometrium was normal for the phase of menstrual cycle.
Laparoscopy: Uterus was unicornuate with well-developed right horn and a non-communicating left sided rudimentary horn. Right fallopian tube and ovary were absent with the presence of surgical staplers and adhesions to pelvic side wall indicative of previous surgery. Left ovary was normal in shape and position but smaller in size. Left fallopian tube was normal in course and caliber with its origin from rudimentary horn [Figure 3a and b].

- (a) Laparoscopic image showing left side rudimentary horn, round ligament, left tube and left ovary. (b) Laparoscopic image showing right side well-developed horn with surgical staplers and absent right adnexa
Genetic analysis showed normal female karyotype (46, XX), and subsequent intravenous pyelogram demonstrated a normal urinary tract.
The decision for in vitro fertilization (IVF) was taken with explained prognosis for poor ovarian response. As the patient was willing for her own genetic child and considering her young age with AFC of 3–5 in left ovary, the patient was started stimulation with human menopausal gonadotropin 450 IU/day from day 2 of her menstrual cycle. After 8 days of maximal stimulation, only one follicle of 10 mm was seen in left ovary. The poor prognosis explained to the couple, and the cycle was canceled. After informed consent, the patient was enrolled for IVF with oocyte donation. She was started with estradiol valerate 6 mg/day from day 2 of her menstrual cycle for endometrial preparation. Donor oocytes were inseminated with husband’s sperms and 2 compaction stage (day 4), grade A embryos were transferred in a trilaminar endometrium of 8.7 mm. Luteal phase support with vaginal micronized progesterone 800 mg/day and estradiol valerate 6 mg/day was prescribed. Serum beta human chorionic gonadotropin (β HCG) on 15th day post-embryo transfer was 2175 mIU/mL. Obstetric scan after 2 weeks revealed a single intrauterine gestational sac with fetal pole and cardiac activity. The luteal phase support was continued till 12th week of gestation. On her dual marker test, there was high risk for Trisomy 21 (1:109), Nuchal translucency 0.9 mm, crown rump length (CRL) 57 mm, for which she underwent amniocentesis at 17th week along with anomaly scan. The results of amniocentesis and anomaly scan were reassuring. At 29 weeks, she was given antenatal corticosteroid prophylaxis. At 34 weeks, her obstetric scan revealed a mild asymmetric intrauterine growth restriction (IUGR); hence a serial growth monitoring was in practice till 37 weeks. At 37 weeks and 4 days, she started having uterine contractions. After examination, decision for cesarean section was taken. She delivered a healthy female child weighing 2184 g with an Apgar score of 9, 9, 9, head circumference of 33 cm and length of 43 cm. Postoperative period was uneventful. Both mother and baby were discharged in healthy condition.
DISCUSSION
In this case, there was unicornuate uterus with non-communicating rudimentary horn. Right adnexa had been surgically removed; left adnexa was present but with diminished ovarian reserve. The patient was left with uterus on one side and adnexa on other side; hence IVF became the only option for conception, but only one ovary with serum AMH level of 0.1 ng/mL posed a great challenge. The women with single ovary have a little reduced ovarian reserve, mainly because of the reduced number of primordial follicles, because they have no compensatory mechanism for the loss of one ovary.
The possible etiologies for diminished ovarian reserve in this case could be surgical, embryological or ischemic event or some genetic mechanism. Previous laparoscopic salpingo-oophorectomy for an adnexal mass at the age of 16 years according to the history given by the patient becomes the obvious culprit at first instance. There may be some surgical insult to the vascular supply of left adnexa during the surgery, resulting in diminished ovarian reserve. In a previous study, there was higher basal FSH concentrations and poor response to ovarian stimulation in women after unilateral oophorectomy; more importantly, this was not age related effect.[7] In absence of histopathological examination (HPE) of surgically removed adnexal mass, it is difficult to conclude if this is a case of unilateral hypoplasia of the ovary or is the case of bilateral ovarian hypoplasia. It is theoretically possible that the ovary that was removed also had poor antral follicular count.
Embryological theory points toward an association between the development of urogenital ridge and mullerain ducts although the exact cause and incidence are not known. There is probably inadequate vascular supply to the caudal region of mullerian duct leading to aberrant signaling of autocrine and paracrine pathways resulting in gonadal dysgenesis.[8] Absence of renal or any other congenital anomaly in our case makes the embryological hypothesis less likely. Kives et al. reported that women with mullerian anomalies might be more prone to ovarian torsion due to abnormal anatomic connections between the ovary and pelvic sidewall.[9] The presence of rudimentary horn can also contribute to the disturbed vascular supply to ipsilateral ovary leading to hypoplasia. The possibility of any underlying genetic condition cannot be ruled out.
Unicornuate uterus is generally associated with poor obstetric performance with higher frequencies of recurrent first and second trimester abortions, preterm deliveries, fetal malpresentations, intrauterine growth retardation, and increased cesarean delivery rate. The reasons behind such outcomes can be diminished muscle mass, abnormal vascular supply and cervical incompetence. Although several studies have suggested a benefit of placement of prophylactic cervical cerclage in all antenatal patients with unicornuate uterus, but the Royal College of Obstetricians and Gynaecologists (RCOG) guidelines advise against it (level B recommendations).[10] Hence we did not place cervical cerclage in our patient and the pregnancy continued well till term. The reported live birth rate in unicornuate uterus is 49.9%,[11] and our case further strengthens the possibility of reasonable obstetric outcome in the patients with unicornuate uterus.
CONCLUSION
We searched the literature for any syndromic association of unicornuate uterus with non-communicating rudimentary horn with diminished ovarian reserve along with strabismus but could not find any. Further research and reporting of similar cases along with genetic testing might help to find one in future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We express gratitude to the patient who gave consent to publish this case report. The authors are thankful to all the staff members for their co-operation. Dr. Ajay Jain is appreciated for his generous help and constant inspiration.
REFERENCES
- The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions. Fertil Steril. 1988;49:944-55.
- [Google Scholar]
- Uterine anomalies: How common are they, and what is their distribution among subtypes? J Reprod Med. 1998;43:877-87.
- [Google Scholar]
- An incidental finding of unicornuate uterus with unilateral ovarian agenesis during cesarean delivery. Arch Gynecol Obstet. 2007;276:91-3.
- [Google Scholar]
- A case of unicornuate uterus with ipsilateral ovarian and renal agenesis. Fertil Steril. 2006;85:750.e1-4.
- [Google Scholar]
- Unilateral ovarian hypoplasia − A report of two cases. Open J Obstet Gynecol. 2012;2:69-72.
- [Google Scholar]
- WHO Laboratory Manual for the Examination and Processing of Human Semen (5th). Geneva: WHO Press; 2010. ISBN 978 92 4 154778 9.
- Significance of basal follicle stimulating hormone levels in women with one ovary in programme of in vitro fertilization. Fertil Steril. 1992;57:835-9.
- [Google Scholar]
- Unilateral ovarian agenesis: Report of three cases and review of the literature. Arch Gynecol Obstet. 2003;268:57-60.
- [Google Scholar]
- Mullerian agenesis and ovarian torsion. A case report and review of literature. J Pediatr Surg. 2005;40:1326-8.
- [Google Scholar]
- Cervical Cerclage. Green-Top Guideline No. 60. London: RCOG; 2011. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg60.







