Translate this page into:
Effect of the endometriomas on ovarian stimulation and pregnancy rate on assisted reproductive outcomes
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Endometriosis is a disease known to be detrimental to fertility. Women with endometriosis, and the presence of endometrioma, may require assisted reproductive technologies to achieve a pregnancy.
Aim:
Our aim was to evaluate the effect of endometriosis and the presence of an endometrioma on outcomes of conventional in vitro fertilization/intra-cytoplasmic sperm injection (ICSI).
Materials and Methods:
The study group consisted of 45 infertile women with either unilateral or bilateral ovarian endometrial cysts of less than 3 cm. The control group consisting of 50 patients with mild male factor infertility was candidate for ICSI treatment during the same time period as the study groups. Both groups were compared for number of oocytes retrieved, grades of oocytes, as well as embryo quantity and quality.
Results:
Our findings showed similar follicle numbers, good embryo grades (I or II) and pregnancy rates in the compared groups. However, patients with endometriosis had higher gonadotropin consumption than the control group. The mean number of retrieved oocytes in patients with endometriosis was significantly lower than control group (P < 0.0001). The numbers of metaphase II (MII) oocytes were significantly lower in patients with endometriosis as compared to the control group 6.11 ± 2.92 vs. 9.32 ± 4.71, respectively (P = 0.0002). In patients with unilateral endometriosis, there were significant differences in terms of fertilization rate, retrieved oocyte and MII oocyte between the normal and involved ovaries; P < 0.5.
Conclusion:
The endometriomas group had a significantly poorer ovarian response and required significantly more ampoules of follicle-stimulating hormone per cycle. They showed poor ovarian response with lower total numbers of retrieved oocytes and lower MII oocytes during the stimulation phase; however, it does not affect the quality of embryos and pregnancy rate per patient.
Keywords
Endometrioma
endometriosis
IVF
ovarian reserve
pregnancy rate
INTRODUCTION
Endometriosis is a common cause of infertility. At present, approximately 20% to 35% of all patients undergoing in vitro fertilization (IVF) are diagnosed with endometriosis[1,2] among who about 30% to 40% suffer from endometriomas.[3,4] The impact of endometriomas on assisted reproductive technologies results is a controversial issue. A previous meta-analysis[5] has shown reduced pregnancy rates in women with endometriomas who underwent IVF treatments when compared to patients with other infertility causes. However, other studies have not confirmed this finding.[6,7,8] In addition, some studies have shown that endometriomas could adversely affect the number of oocytes retrieved,[7,9] oocyte quality, fertilization rate,[5,10] embryo quality and implantation rate.[9,11,12] Kumbak et al.[13] have also reported poor embryo quality in patients with endometriosis; yet, there have been no effect on pregnancy rate. Other studies also found no adverse effect of endometriomas on pregnancy success rates.[14,15,16]
Due to these conflicting results, the optimum management of endometriomas in IVF/intra-cytoplasmic sperm injection (ICSI) cycles is not clear.[14,17] Some authors believe that endometriomas should be removed before the IVF cycle[18]; however, others have shown that excision of an endometriomas before an IVF cycle is likely to lead poor responses to ovarian stimulation and to impact fertility outcomes.[19,20]
The focus of the present study was to evaluate the effect of endometriomas on ovarian response and IVF/ICSI outcomes when compared to patients with mild male factor infertility.
MATERIALS AND METHODS
This cohort study was performed at MAGS Medical and Research Center, West Bengal, India. We recruited a total of 95 women who were candidates for IVF/ICSI and fresh embryo transfers.
The study group consisted of 45 infertile women with either mono-lateral or bilateral ovarian endometrial cysts of less than 3 cm, based upon transvaginal sonographic diagnosis with diffuse low-level echoes without neoplastic or acute haemorrhage features. Patients had no histories of any ovarian surgeries. All ultrasound tests were performed by two expert technicians. Technicians performed transvaginal ultrasounds between days 1 and 8 of the cycle, before starting ovarian stimulation. The location and dimension of the endometriosis were recorded at this time.
Patients with endometriosis larger than 3 cm underwent endometriotic cystectomy, via laparoscopic surgery. These patients were not included at the study. There was no patient with cystectomies, defined as a laparoscopic surgery applied for women with small ovarian endometriosis.
The control group consisting of 50 patients with mild male factor infertility was candidate for ICSI treatment during the same time period as the study groups. Mild male factor infertility was defined as the presence of at least 1 million motile sperm after processing. All patients in both groups had indications for IVF/ICSI treatments, without any previous attempts.
Exclude the patients for both groups who were (1) previous history of any systematic disease or malignancy, (2) basal follicle-stimulating hormone (FSH) more than 15 mIU/ml, (3) history of three or more unsuccessful IVF attempts and (4) ovarian endometriosis less than 3 cm.
The study was approved by the local ethics committee. A written informed consent was obtained from all individuals before participation. All patients received the long protocol with a gonadotropin-releasing hormone (GnRH) agonist (0.25 mg/0.5 ml) for pituitary desensitization from the mid-luteal phase of the previous cycle to the day of hCG injection. We began gonadotrophin stimulation 14 days after subcutaneous GnRH agonist injection with daily dose of 150 IU of recombinant FSH. The dose was modified based on monitoring of serum oestradiol (E2) and ultrasound evaluation. When the level of serum oestradiol was >600 pg/ml and two or more leading follicles had mean diameters of >18 mm in two dimensions, 10,000 U of human chorionic gonadotropin were given. Transvaginal sonographically guided ovum retrieval was performed under general anaesthesia 34 h following human chorionic gonadotropin (hCG) administration. The number of dominant follicles on the day of hCG injection and the number of oocytes retrieved from ovaries of diseased site and normal sites was recorded. The definition of dominant follicle was a greatest diameter of >16 mm, or a mean diameter of >14 mm for all follicles. Transcervical or transfallopian embryo transfer was conducted 48 to 72 h after oocyte retrieval. The luteal phase was supported by three injections of 2500 U of hCG every 3rd day, beginning 48 h after oocyte retrieval, or progesterone supplementation, beginning the day of ovum pick up until the day of β-hCG assay. Clinical pregnancy was documented by the presence of an intrauterine gestational sac on transvaginal ultrasound 4 weeks after embryo transfer.
Metaphase II (MII) oocytes were injected using ICSI procedure. Normal fertilization was confirmed when two distinct pro-nuclei were present within 16 to 18 h following oocyte injection.
In ICSI cycles, cumulus-enclosed oocytes were treated with 0.1% hyaluronidase, and the cumulus cells were mechanically removed by pipetting. Oocyte maturation stage and morphology were assessed under an inverted microscope (Nikon, Nikon Eclipse Ti2, Japan) at ×400 magnifications. Oocytes were classified as MII oocyte (mature oocyte), metaphase I oocyte or prophase I oocyte. Good-quality cleaved embryos[21] were transferred 2 to 3 days after oocyte retrieval.
The initial dose, total dose and days of gonadotropin, endometrium thickness and concentration of oestradiol and progesterone on the days of hCG injection were recorded. Numbers of retrieved eggs, rate of cleavage, numbers of embryos grades I and II obtained, scores of the transferred embryos, as well as rates of clinical pregnancy and implantation were calculated.
Main outcome measures
Our primary outcomes were clinical pregnancy rate, mean number of oocyte retrieved, fertilization rate, implantation rate, antral follicle count, total stimulating hormone dose and any rates of adverse effects such as cancellation and associated complications during the IVF/ICSI treatment.
Statistical analysis
Analysis was performed using the SPSS (version 20.0; SPSS Inc., Chicago, Illinois, USA) statistical software. Between-group differences of normally distributed continuous variables were assessed by Student’s t test, whereas the Mann–Whitney U test was used for the abnormal distributed data.
Significant differences were evaluated by the Chi-square test to compare non-continuous variables. In inter-group comparison, the paired t test analysis and Wilcoxon signed-rank test were applied for patients with unilateral endometriosis and for non-parametric cases, respectively. Data were expressed as mean ± standard deviation. Statistical significance was considered when P < 0.05.
RESULTS
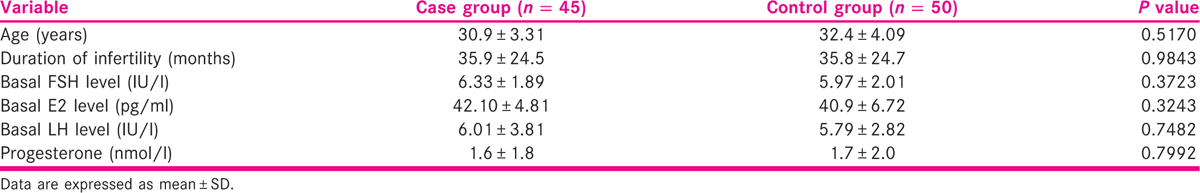
The baseline characteristics including age, duration of infertility and basic concentrations of E2 and FSH level were similar between two groups [Table 1]. The numbers of MII oocytes were significantly lower in patients with endometriosis as compared to the control group 6.11 ± 2.92 vs. 9.32 ± 4.71, respectively (P = 0.0002) [Table 2].

The thickness of the endometrium, follicle numbers and good quality embryos (grade I or II) were also comparable between the two groups (P > 0.05). Both groups had similar implantation and pregnancy rates [Table 2]. However, patients with endometriosis had higher gonadotropin consumption as compared with the control group (35.04 ± 10.11 vs. 22.92 ± 8.32; P < 0.0001).
In patients with unilateral endometriosis, we compared outcomes between the affected ovary and healthy contralateral ovary. There were significant differences in terms of fertilization rate, retrieved oocyte and MII oocyte between the normal and involved ovaries; P < 0.5 [Table 3].

DISCUSSION
In the present study, the numbers of MII oocytes were significantly lower in endometriosis patients than the controls. These results were consistent with previous investigations that found a lower ovarian response to gonadotropin stimulation in patients with endometriosis.[13,22] Al-Azemi et al.[23] have reported that endometriomas led to a decreased response to gonadotropins, as reflected by the smaller number of retrieved oocytes, which was also shown in our study. Pellicer et al.[24] have demonstrated that endometriosis caused poor-quality oocytes and embryos with decreased ability for implantation. Different mechanisms such as changes in autoimmune factors, cytokines or production of growth factors, increased rate of granulosa cell apoptosis and decreased steroid levels were considered as negative factors for follicular growth and oocyte maturity in these patients.[25,26] Some previous studies have reported poor IVF-embryo transfer outcomes with endometriosis.[9,11,12] We could not find any negative impact of endometriomas on clinical pregnancy and implantation rates. Some researchers have also shown that the existence of endometriosis did not influence embryo implantation and have proposed that the detrimental effects were limited to the fertilization phase.[27] In patients with unilateral endometriosis, the presence of endometriosis at the time of aspiration did not compromise our ICSI outcomes. It seems that in women with unilateral disease, the contralateral intact ovary compensated for ovarian function and fertility potential.[14] In the present study, we did not include patients who had surgery for their endometriosis. Additional studies are required to evaluate the effect of surgery.
CONCLUSION
Despite the lower response to gonadotropins in endometriosis patients, the rates of pregnancy and implantation rates, embryo quality and fertilization of MII oocytes were not affected by the presence of the endometriosis. It seems that endometrial receptivity in two groups was similar.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
ACKNOWLEDGEMENTS
The authors gratefully thank all the couples participating in the study.
REFERENCES
- The prevalence of endometriosis in pre-menopausal women undergoing gynecological surgery. Clin Exp Obstet Gynecol. 1994;21:195-7.
- [Google Scholar]
- Endometriosis: Pathogenetic implications of the anatomic distribution. Obstet Gynecol. 1986;67:335-8.
- [Google Scholar]
- Coagulation or excision of ovarian endometriomas? Am J Obstet Gynecol. 2003;188:606-10.
- [Google Scholar]
- Women with advanced-stage endometriosis and previous surgery respond less well to gonadotropin stimulation, but have similar IVF implantation and delivery rates compared with women with tubal factor infertility. Fertil Steril. 2007;88:1568-72.
- [Google Scholar]
- Impact of ovarian endometrioma on oocytes and pregnancy outcome in in vitro fertilization. Fertil Steril. 2005;83:908-13.
- [Google Scholar]
- Centers for disease control and prevention (CDC). Assisted reproductive technology surveillance − United States, 2005. MMWR Surveill Summ. 2008;57:1-23.
- [Google Scholar]
- Effects of endometriomas on ooccyte quality, embryo quality, and pregnancy rates in in vitro fertilization cycles: A prospective, case-controlled study. J Assist Reprod Genet. 1998;15:193-7.
- [Google Scholar]
- Is the endometrium or oocyte/embryo affected in endometriosis? Hum Reprod. 1999;14(Suppl 2):77-89.
- [Google Scholar]
- Patients with stages III and IV endometriosis have a poorer outcome of in vitro fertilization-embryo transfer than patients with tubal infertility. Fertil Steril. 1999;72:1107-9.
- [Google Scholar]
- Outcome of IVF in patients with endometriosis in comparison with tubal-factor infertility. J Assist Reprod Genet. 1998;15:530-4.
- [Google Scholar]
- In vitro fertilization in normoresponder patients with endometriomas: Comparison with basal simple ovarian cysts. Gynecol Obstet Invest. 2008;65:212-6.
- [Google Scholar]
- Should endometriomas be treated before IVF-ICSI cycles? Hum Reprod Update. 2006;12:57-64.
- [Google Scholar]
- Effects of ovarian endometrioma on the number of oocytes retrieved for in vitro fertilization. Fertil Steril. 2011;95:525-7.
- [Google Scholar]
- Endometriosis and assisted reproduction: The role for reproductive surgery? Curr Opin Obstet Gynecol. 2006;18:374-9.
- [Google Scholar]
- Endometrioma undergoing laparoscopic ovarian cystectomy: Its influence on the outcome of in vitro fertilization and embryo transfer (IVF-ET) J Assist Reprod Genet. 2005;22:329-33.
- [Google Scholar]
- Effect of endometrioma cystectomy on IVF outcome: A prospective randomized study. Reprod Biomed Online. 2006;12:639-43.
- [Google Scholar]
- Does laparoscopic excision of endometriotic ovarian cysts significantly affect ovarian reserve? Insights from IVF cycles. Hum Reprod. 2003;18:2450-3.
- [Google Scholar]
- Effect of endometriosis on IVF/ICSI outcome: Stage III/IV endometriosis worsens cumulative pregnancy and live-born rates. Hum Reprod. 2005;20:3130-5.
- [Google Scholar]
- Ovarian response to repeated controlled stimulation in in-vitro fertilization cycles in patients with ovarian endometriosis. Hum Reprod. 2000;15:72-5.
- [Google Scholar]
- The pathophysiology of endometriosis-associated infertility: Follicular environment and embryo quality. J Reprod Fertil Suppl. 2000;55:109-19.
- [Google Scholar]
- Immune abnormalities in endometriosis compromising fertility in IVF-ET patients. J Reprod Med. 1999;44:458-64.
- [Google Scholar]
- Exploring the mechanism of endometriosis-related infertility: An analysis of embryo development and implantation in assisted reproduction. Hum Reprod. 1995;10(Suppl 2):91-7.
- [Google Scholar]
- Results of in vitro fertilization in patients with endometriomas: Is surgical removal beneficial? Am J Obstet Gynecol. 2004;191:597-607.
- [Google Scholar]







