Translate this page into:
Role of daily ejaculation for four consecutive days in improving sperm DNA fragmentation index
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Semen analysis is the gold standard for determining male partner fertility but it does not provide any information about the genetic make-up of the sperm, which is essential for normal embryo development. High sperm DNA fragmentation is also found in men with normal semen parameters. Sperm with high DNA damage leads to nuclear instability in the embryo, resulting in developmental arrest, implantation failure, higher miscarriage rate, genetic mutations causing abnormalities in the offspring and increased susceptibility to childhood cancers. European Society for Human Reproduction and Embryology (ESHRE 2017) guidelines recommend sperm DNA fragmentation testing for men whose partners experience recurrent pregnancy loss. In 25th annual meeting of ESHRE it was discussed that daily sex helps to reduce sperm DNA damage and improve fertility. The basis for this is that daily ejaculations reduce the exposure of sperms to reactive oxygen species in testicular ducts and epididymis; hence less DNA damage and improvement in DNA fragmentation index. Extrapolating this, it is hypothesized that a reduction in DFI will be observed when analysing semen obtained after daily ejaculation for four days.
Aim:
The aim of the study is to evaluate the role of daily ejaculation for four consecutive days in improving the sperm DNA fragmentation index (DFI).
Materials and Methods:
Out of 170 semen samples, 65 patients had DFI of > 30% in a routine workup of male factor in an infertile couple and were recruited. Of these 56 opted for participating in this study. The initial semen sample was collected after an abstinence of 2-3 days. These patients were then asked to ejaculate daily for four consecutive days. During this period, no medication or any lifestyle modification was advised to these patients. Repeat semen sample was then collected on fifth day and DNA fragmentation index was calculated using the sperm chromatin dispersion (SCD) test.
Results:
The mean age of the patients was 35.52 years (range 29–50 years). The Indications for raised DFI were: age > 35 years (41%), BMI >25 (30.35%), defective spermatogenesis (31%), diabetes (5.35%), varicocoele (5.35%), smoking (32.14%). The mean DFI in the initial sample was 57.36 ± 17.54 and the mean DFI in the repeat sample was 32.33 ± 21.62. The reduction in the DFI was statistically significant with a P-value of <0.0001. A decrease in the sperm count after daily ejaculations was also observed but the difference was not statistically significant (45.05 ± 31.47 vs 41.38 ± 33.72; P-value = 0.07). No statistically significant difference was seen in the sperm motility (45.59 ± 15.47 vs 46.5 ± 14.33) and sperm morphology (11.11 ± 13.17 vs 10.75 ± 12.94) after repeated ejaculations.
Conclusion:
Daily ejaculations for four consecutive days by patients showing high sperm DNA damage is a cost-effective method of reducing DFI without compromising other semen parameters.
Keywords
DNA fragmentation index
male infertility
short abstinence
sperm chromation dispersion test
INTRODUCTION
Male factor accounts for a total of 30%–50% infertility cases and is mainly due to the defects at the level of sperms.[1] Till date semen analysis remains the gold standard test for assessing the fertility potential of male partner. But, it does not provide any information about the genetic make-up of the sperm, which is the most important determinant for normal embryo development. Sperm with high DNA damage causes nuclear instability in the embryo resulting in developmental arrest of the embryo, implantation failure, higher miscarriage rate in both natural and IVF/ICSI conceptions.[2,3] Damaged sperm DNA also leads to cell degeneration and mutations, causing abnormalities in the offspring and increased susceptibility to childhood cancers.[4]
Integrity of sperm DNA is determined by DNA fragmentation index (DFI) i.e percentage of sperms with fragmented DNA.[5] Although sperm DNA damage is more in infertile men as compared to fertile men, high sperm DNA fragmentation is also found in men with normal semen parameters.[2,6,7] Hence it becomes necessary to know the DNA status of the sperm along with other semen parameters.
Sperm DNA damage can occur due to: (i) Deficiencies in recombination during spermatogenesis and defective protamine packaging.[8,9] (ii) Production of reactive oxygen species (ROS) by the immature sperms and/or leukocytes during their co-migration from the seminiferous tubules to the epididymis.[9,10] (iii) Presence of ROS in seminal fluid after ejaculation.[9,10] The numerous factors resulting in high sperm DFI are divided into pre-testicular, testicular and post testicular causes.[9,11]
Pre-testicular: Age >35 years, smoking, high BMI, diabetes mellitus, cytotoxic effects of chemotherapy and radiotherapy.
Testicular: Varicocoele, increased scrotal temperature (hot baths, fever, tight clothes, cryptorchidism), genitourinary infections (c. trachomatis, mycoplasma), increase in immature germ cell concentration, leukocytospermia.
Post testicular: obstruction at the level of epididymis, vas deferens.
Most commonly employed tests for sperm DNA fragmentation measurement are Sperm Chromatin Structure Assay (SCSA), TUNEL Assay, Comet Assay, Sperm Chromatin Dispersion Test (SCDt), DNA Breakage Detection-FISH (DBD-FISH) test, Single-cell pulsed-field gel electrophoresis technique.[9,12]
European Society for Human Reproduction and Embryology (ESHRE 2017) recommends sperm DNA fragmentation testing for men whose partners experience recurrent pregnancy loss.[13] In 25th annual meeting of ESHRE it was discussed that daily ejaculation for seven days helps to reduce sperm DNA damage and improve fertility.[14] The basis for this is that daily ejaculations reduce the exposure of sperms to reactive oxygen species in testicular ducts and epididymis; hence less DNA damage and thus improvement in DNA fragmentation index.
Extrapolating this, it is hypothesized that a reduction in DFI will be observed when analysing sperms obtained after daily ejaculation for four days.
AIM
The aim of the study is to evaluate the role of daily ejaculation for four consecutive days in improving the sperm DNA fragmentation index (DFI).
MATERIALS AND METHODS
The present study was conducted between January 2019–December 2019. Out of a total of 170 semen samples, 65 patients were found to have a high DFI. Out of these, 56 men opted for participating in this study. These fifty-six men with increased sperm DNA damage, indicated by raised DFI of > 30% in a routine work-up of male factor in an infertile couple were recruited. The initial semen sample was collected after an abstinence of 2–3 days, as per the hospital protocol. Semen collection was done in the sample collection room of the centre by masturbation. DFI higher than or equal to 30% was taken as the cut off. The repeat sample was collected on the fifth day of the first sample, meanwhile patients were asked to ejaculate daily for four consecutive days. During this period, any medication or any lifestyle modification was not advised to them. Repeat semen sample was collected in the same way. Samples were immediately transferred to the adjoining laboratory. After complete liquefaction, semen analysis determining semen volume, viscosity, sperm concentration, motility was performed using WHO 2010 guidelines. Adopting strict Kruger’s criteria sperm morphology was assessed. Neat semen samples were subjected to SCDt (Sperm chromatin dispersion test) (Figure 1) for DNA fragmentation index calculation.
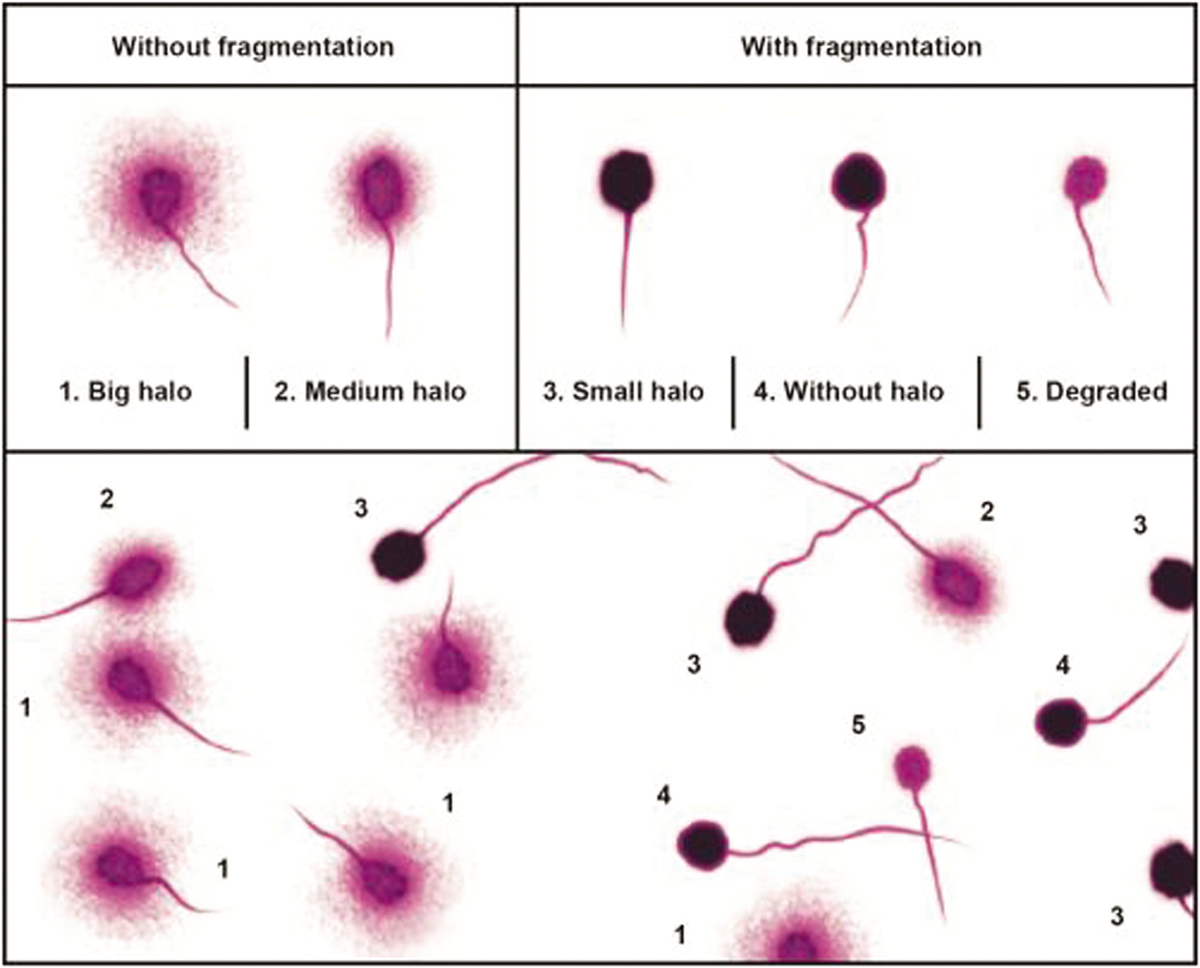
- Showing Interpretation of sperm chromation dispersion test (SCDt)
STATISTICAL ANALYSIS
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected then non parametric test was used. Quantitative variables were compared using paired t test/Wilcoxon signed rank Test (when the data sets were not normally distributed) between pre and post. A P value of <0.05 was considered statistically significant. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
RESULTS
The mean age of the patients was 35.52 ± 4.77 years (range 30–50 years) with mean BMI of 30.05 ± 31.47 [Table 1].

Maximum number of patients, 57.14% (n = 32) were working in multinational companies followed by private and government sector respectively [Table 2].

There was no incidence of fever in any of the patients in last 3 months prior to producing the semen samples.
Table 3 depicts the causes for high DNA fragmentation index. Age > 35 years and BMI > 25 was seen in 41.06% and 30.35% patients respectively. Raised DFI with abnormal sperm parameters was present in 30.3% (n = 17) patients. 5.35% patients were diabetic and varicocoele as a cause of raised DFI was seen in 5.35% men. Smoking as an independent risk factor was found in 32.14% patients who smoked 4-5 cigarettes per day on an average. 19.64% men had more than one above-mentioned causal factor.

Mean DFI in the initial sample was 57.36% (range 33%–95%), which dropped to a mean value of 32.33% (range 5–56%) after daily ejaculations for four consecutive days [Table 4].

In the repeat sample 57.1% patients (n= 32) had a drop in DFI to <30%, while 21.4%, 10.7% and 10.7% patients had repeat DFI between 31%–40%, 41%–50%, 51%–60% respectively. None of the patients had DFI > 56% in the repeat sample, while in the initial sample extremely high DFI values were noted [Table 5].

Although there was a significant improvement in DFI after daily ejaculation, however, 37.5% men showing a drop in DFI had DFI values above 30%, while 5.35% men exhibited an increase in DFI [Table 6].

No statistically significant differences were observed in total sperm concentration, total sperm motility and morphology [Table 7].

DISCUSSION
In the present study, short abstinence period in the form of daily ejaculations for four days, resulted in a significant drop in the mean DFI by 25% without any significant change in other sperm parameters.
High BMI, diabetes, presence of varicocoele, history of smoking, defective spermatogenesis were the common factors for raised DFI in our study. Petersen[15] and Belloe[16] et al. documented that oxidative stress and disordered apoptosis cause significant increase in DFI after 35 years of age. However, majority of the men (58.92%) with high DFI in our study were < 35 years of age. The reason for raised DFI in these patients was presence of other factors causing increased DNA damage. Obesity[17] and diabetes[18] are associated with various endocrinological factors that cause defective spermatogenesis and negatively influence sperm DNA integrity.
Lifestyle, working conditions, environment have a bearing on DNA make-up and a positive correlation with abnormal DFI.[18] In the present study maximum men (57.14%) were working in multinational companies involving long working hours, sitting job, prolonged use of laptops with internet, causing epigenetic changes in the sperm DNA. Studies[19,20] have documented that varicocoele results in increased production of immature sperms. ROS released from the immature sperms, can damage the mature sperm DNA. Sperm DNA integrity is influenced by smoking because of the deleterious effects of nicotine on the rapidly dividing spermatogenic cells.[21]
Different DFI cut off values have been proposed. Greening et al.[14] defined DFI <15% for excellent sperm quality and > 29% DFI as poor quality sperm. Similarly most authors considered sperm DNA fragmentation index of > 30% by SCDt (Sperm chromatin dispersion test) to reflect a poor fertility potential.[22,23]
Many studies have been conducted in past to evaluate the role of short abstinence periods in improving sperm DFI but conflicting conclusions have been drawn.[24,25,26] Comar Venessa et al.[27] conducted a study on 2458 men and concluded that as the abstinence period expands, sperm DFI increases. Literature suggests that prolonged epididymal storage changes the thiol disulphide bonds in protamines causing instability of sperm DNA.[11]
Similar to our study, Gosalvez et al.[23] also noted 25% drop in mean DFI in neat semen sample collected after four daily ejaculations, but the difference was that their study was conducted on normozoospermic males while our study included oligozoospermic men as well.
In the present series 57.14% patients showed an improvement in the DFI, with DFI declining to < 30% in the repeat sample. Isabel et al.[11] had compared the DFI values using one-day abstinence protocol and found that DFI dropped to <30% in 81% patients in the repeat sample. The variation in the results could be due to difference in the sample size. Greening et al.[14] observed a mean DFI drop from 34% to 26% in 118 men after daily ejaculations for 7 days. 81% men had DFI <23% in repeat sample. The aforementioned studies have included men with both normal and abnormal semen parameters.
In our study 37.5% (n = 21) patients showed a decrease in DFI by shortening the abstinence period but the value remained >30%. Table 8 shows that these patients had either defective spermatogenesis (OATS, oligozoospermia) or presence of multiple risk factors causing high sperm DNA damage due to increased production of ROS. De Jonge et al.[28] reported similar findings in their study and concluded that short abstinence time can decrease the sperm DNA denaturation occurring at the time of epididymal storage but cannot improve the deficiencies in DNA caused during defective spermiogenesis. In Patients with multiple causative factors for high DNA damage, repeated ejaculations do show improvement in the DFI by minimizing the interaction of sperms with ROS, but since the relative amount of ROS is more, DFI remains >30%.

In contrast to the proposed hypothesis of drop in DFI after repeated ejaculations, 5.35% (n = 3) men in our study showed an increased DFI in the repeat sample [Tables 6, 9].

Since the rise was not significant, we presume that it could have been due to subjective variation while performing the SCDt. Another reason could be the presence of multiple risk factors, where daily ejaculations might not have improved the DFI. It has been urged that frequent ejaculations offer inadequate time for nuclear maturation of spermatozoa, which makes them highly prone to DNA damage. The presence of immature sperms partly explains the rise in DFI >30% after daily ejaculations.[24]
Greeting et al.[14] reported 19% patients with 10% increase in DFI after daily ejaculations for 7 days. Mayorga-Torres et al.[29] also found an increasing trend in DFI in three subsequent samples after extremely short abstinence period of 2 hours each. Very small sample size (n = 3) was the limitation of their study. Hence, larger studies are needed to establish the reason for increase in DFI after short abstinence period.
In the present study we observed a decrease in total sperm concentration [Table 7], which was an expected finding but the difference was not statistically significant. Literature suggests that there is an increase in total number and concentration of spermatozoa with increase in the abstinence period.[30,31,32]
In agreement with the previous studies,[31,32] there was no significant difference in the normal sperm morphology after abstinence for 2-3 days vs. daily ejaculations for 4 days. Bahadur et al.[33] however reported that significant improvement in normal sperm forms was seen with extremely short abstinence period of 40 minutes.
Considering the total sperm motility, which is the critical factor in determining the functional sperm capacity, we had not observed any significant difference in total sperm motility and fast progressive motility in the repeat sample [Table 10]. Skandhan et al.[34] suggested that prolonged abstinence exposes the stored spermatozoa to various quiescence factors. Daily ejaculations decrease the concentration of these factors, thus improving sperm motility. However, no such conclusion can be drawn from our study.

Numerous studies have been conducted in the past with an aim to device the methods for decreasing the sperm DNA damage. Several studies support the use of antioxidants but the results are conflicting.[35,36,37] Moreover, use of antioxidants adds to the treatment cost. Role of antibiotics have been advocated in cases of leucocytospermia.[38] Testicular biopsy is an invasive technique while MACS (magnetic activates sperm sorting) is expensive. Before planning testicular sperm retrieval in high DFI cases, this technique can be adopted as a non −invasive method for healthy sperm selection.
CONCLUSION
Daily ejaculations for four consecutive days significantly improve sperm DNA fragmentation index without affecting other sperm parameters. This approach proves to be simple, cost effective, with good patient compliance in improving male fertility potential.
Strength: 1) Single centre study. 2) This intervention has evaluated within-subject variation in sperm parameters and DFI after daily ejaculations.
Limitation: 1) Small sample size
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Associations of sperm DNA fragmentation with lifestyle factors and semen parameters of Saudi men and its impact on ICSI outcome. Reproductive Biology and Endocrinology. 2018;16:49-54.
- [Google Scholar]
- Sperm chromatin damage impairs human fertility. The Danish first pregnancy planner study team. Fertil Steril. 2000;73:43-50.
- [Google Scholar]
- Sperm chromation structure assay parameters as predictors of failed pregnancy following assisted reproductive techniques. Hum Reprod. 2000;8:1717-22.
- [Google Scholar]
- Long term effects of mouse intracytoplasmic sperm injection with DNA fragmented sperm on health and behaviour of adult offspring. Biol Reprod. 2008;78:761-72.
- [Google Scholar]
- Successful outcomes achieved in assisted reproduction cycles using sperm with high levels of high DNA stainability. Sys Biol Reprod Med. 2015;61:293-9.
- [Google Scholar]
- DNA integrity in human spermatozoa: relationship with semen quality. J Androl. 2000;21:33-44.
- [Google Scholar]
- Prevalence of abnormal sperm DNA denaturation in fertile and infertile men. Urology. 2002;60:1069-72.
- [Google Scholar]
- Increased DNA damage in sperm from leukocytospermic semen samples as determined by the sperm chromatin structure assay. Fertil Steril. 2002;78:319-20.
- [Google Scholar]
- Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. Int J Mol Sci. 2012;13:14026-52.
- [Google Scholar]
- Differential production of reactive oxygen species by subsets of human spermatozoa at different stages of maturation. Hum Reprod. 2001;16:1922-30.
- [Google Scholar]
- One abstinence day decreases sperm DNA fragmentation in 90% of selected patients. J Assist Reprod Genet. 2013;30:1211-8.
- [Google Scholar]
- Sperm DNA fragmentation: threshold value in male fertility. Hum Reprod. 2005;20:3446-51.
- [Google Scholar]
- Recurrent pregnancy loss 2017:118-20. version 2
- Daily Sex Helps Reduce Sperm DNA Damage And Improve Fertility. Science Daily 2009 July 1
- [Google Scholar]
- The effects of male age on sperm DNA damage: an evaluation of 2, 178 semen samples. JBRA Assist Reprod. 2018;22:323-30.
- [Google Scholar]
- Paternal age and sperm DNA decay: Discrepancy between chromomycin and aniline blue staining. Reprod. Biomed Online. 2009;19:264-9.
- [Google Scholar]
- Impact of body mass index values on sperm quantity and quality. J Androl. 2006;27:450-2.
- [Google Scholar]
- The etiologies of DNA abnormalities in male infertility: an assessment and review. Int J Reprod Biomed (Yazd). 2017;15:331-44.
- [Google Scholar]
- Are varicocoeles associated with increased deoxyribonucleic acid fragmentation? Fertil Steril. 2011;96:1283-7.
- [Google Scholar]
- Effect of varicocoele on chromatin condensation and DNA integrity of ejaculated spermatozoa using cytochemical tests. Androlgia. 2008;40:245-51.
- [Google Scholar]
- Sperm selection by swim-up in terms of deoxyribonucleic acid fragmentation as measured by the sperm chromatin dispersion test is altered in heavy smokers. Fertil Steril. 2007;88:523-5.
- [Google Scholar]
- Relation of mammalian sperm chromatin heterogeneity to fertility. Science. 1980;210:1131-3.
- [Google Scholar]
- Shorter abstinence decreases sperm deoxyribonucleic acid fragmentation in ejaculate. Fertil Steril. 2011;96:1083-6.
- [Google Scholar]
- Influence of ejaculation frequency on seminal parameters. Reprod Biol Endocrinol. 2015;13:1.
- [Google Scholar]
- Increased pregnancy after reduced male abstinence. Syst Biol Reprod Med. 2013;59:256-60.
- [Google Scholar]
- Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005;83:1680-6.
- [Google Scholar]
- Influence of the abstinence period on human sperm quality: analysis of 2, 458 semen samples. JBRA Assist Reprod. 2017;21:306-12.
- [Google Scholar]
- Influence of the abstinence period on human sperm quality. Fertil Steril. 2004;82:57-65.
- [Google Scholar]
- Can a short term of repeated ejaculations affect seminal parameters? J Reprod Infertil. 2016;17:177-83.
- [Google Scholar]
- Abstinence time and its impact on basic and advanced semen parameters. Urology. 2016;94:102-10.
- [Google Scholar]
- Effect of age and abstinence on semen quality: a retrospective study in a teaching hospital. Asian Pac J Reprod. 2014;3:134-41.
- [Google Scholar]
- The effects of short abstinence time on sperm motility, morphology and DNA damage. Andrology. 2013;2:1-5.
- [Google Scholar]
- Semen characteristics in consecutive ejaculates with short abstinence in subfertile males. Reprod Biomed Online. 2016;32:323-8.
- [Google Scholar]
- Hypothesis: epididymis inhibits sperm motility inside male reproductive tract. Med Hypotheses. 2004;62:146-50.
- [Google Scholar]
- ICSI in cases of sperm DNA damage: beneficial effect of oral antioxidant treatment. Hum Reprod. 2005;9:2590-4.
- [Google Scholar]
- A randomised control trial examining the effect of an antioxidant (Menevit) on pregnancy outcome during IVF-ICSI treatment. ANZJOG. 2007;47:216-21.
- [Google Scholar]
- Improvement in sperm DNA quality using an oral antioxidant therapy. Reprod Biomed Online. 2010;18:761-8.
- [Google Scholar]
- Sperm DNA fragmentation in infertile men with genitourinary infection by Chlamydia trachomatis and Micoplasma. Fertil Steril. 2008;90:328-34.
- [Google Scholar]







