Translate this page into:
IFS recommendations for COVID-19 Vaccination COVID-19 before ART
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
INTRODUCTION
The coronavirus pandemic has wreaked havoc on life and healthcare globally. According to WHO database as on 7th June 2021, there have been 173 million confirmed covid19 cases worldwide and 3.7 million deaths. The World Health Organization declared the outbreak a Public Health Emergency of International Concern on 30 January 2020, and a pandemic on 11 March 2020. SARS-CoV-2 is a positive-sense single-stranded RNA virus that is contagious in humans. As described by the US National Institutes of Health, it is the successor to SARS-CoV-1, the virus that caused the 2002–2004 SARS outbreak
India is just recovering from the deadly second wave of the pandemic with more than 28 million confirmed cases and 3.49 lakh deaths.
In these trying times, as societies are gradually trying to return to a state of normalcy, it is also important to consider sexual and reproductive health of people.
Couples seeking conception are particularly distressed and need clear guidelines to help them make decisions about their treatment.
This document of the IFS has been prepared after taking inputs from all the chapter secretaries of the IFS and hence includes insights and common queries addressed by the healthcare providers across the country. It intends to provide both the providers and the patients an overview of covid vaccination in patients desiring fertility in order to help them make an informed choice regarding the vaccination.
THE VIRUS
COVID-19 disease is caused by the virus, SARS CoV2(Severe acute respiratory syndrome coronavirus 2) which is a beta coronavirus. Coronaviruses infect humans, other mammals, and avian species, including livestock and companion animals. Human coronaviruses are capable of causing illnesses ranging from the common cold to more severe diseases such as Middle East respiratory syndrome (MERS, fatality rate ∼34%). SARS-CoV-2 is the seventh known coronavirus to infect people, after 229E, NL63, OC43, HKU1, MERS-CoV, and the original SARS-CoV.
It bears 80% homology to SARS Cov and 50% to MERS.[1]
Each SARS-CoV-2 virion is 50–200 nanometres in diameter.
It is an enveloped positive-sense single stranded RNA virus with four main structural proteins i.e. Spike (S) protein, Membrane (M) protein, Nucleocapsid (N) protein and envelope (E) protein.[2] In SARS-CoV-2, the spike protein, which has been imaged at the atomic level using cryogenic electron microscopy, is the protein responsible for allowing the virus to attach to and fuse with the membrane of a host cell; specifically, its S1 subunit catalyzes attachment, the S2 subunit fusion.
It binds to angiotensin receptor conversion enzyme 2 (ACE2) on host cells for viral entry and with the help of Transmembrane serine proteases 2 (TMPRSS2) is incorporated in host cell wall.[3] Initial spike protein priming by transmembrane protease, serine 2 (TMPRSS2) is essential for entry of SARS‑CoV‑2.] The host protein neuropilin 1 (NRP1) may aid the virus in host cell entry using ACE2. After a SARS‑CoV‑2 virion attaches to a target cell, the cell’s TMPRSS2 cuts open the spike protein of the virus, exposing a fusion peptide in the S2 subunit, and the host receptor ACE2. After fusion, an endosome forms around the virion, separating it from the rest of the host cell. The virion escapes when the pH of the endosome drops or when cathepsin, a host cysteine protease, cleaves it. The virion then releases RNA into the cell and forces the cell to produce and disseminate copies of the virus, which infect more cells.
SARS-CoV-2 produces at least three virulence factors that promote shedding of new virions from host cells and inhibit immune response.
An understanding of the structure of the virus has helped in developing preventive and treatment strategies against it.
The need for vaccination
Impact on reproduction
COVID-19 may influence both male and female steroidogenesis, germ cells and reproductive health.[4] The reproductive system in both sexes has abundant ACE2 receptors and are susceptible to SARS CoV 2 infection. Studies have suggested that downregulation of ACE 2 may cause alteration in follicular development and oocyte maturation affecting their quality and subsequently affecting embryo development. Also increased oxidative stress may have detrimental pro inflammatory effect. Endometrial receptivity may also be altered leading to unfavourable outcomes.[5]
Hajizadeh Malekiand Tartibian conducted a prospective, longitudinal cohort study of 84 men with laboratory-confirmed COVID-19 and 105 men without the disease in Iran. The researchers analyzed changes in angiotensin-converting enzyme 2 (ACE2) activity, markers of inflammation and oxidative stress, apoptotic variables and semen quality, all of which were evaluated at 10-day intervals for up to 60 days. They also had higher levels of reactive oxygen species and lower superoxide dismutase activity compared with healthy controls.
The markers of inflammation and oxidative stress in sperm cells of men with COVID-19 were increased by more than 100% compared with controls, according to the researchers. Sperm concentration was reduced by 516%, mobility by 209% and sperm cell shape was altered by 400%. Although these effects were reported to improve over time — representing “a transient state of male subfertility like those with oligoasthenoteratozoospermia” — the researchers wrote they remained “significantly and abnormally higher in the COVID-19 patients, and the magnitude of these changes were also related to disease severity.”
So couples should be advised to continue with efforts at conception, follow all preventive measures and meanwhile seek vaccination at the earliest.[11] Basigin (BSG) is also one of the most crucial receptors for COVID-19 that mediates its entry to host cells. BSG is expressed not only in the uterus but also in the stroma and granulosa cells of the ovary. BSG may play a role during follicle development, corpus luteum formation and embryo implantation.
In men viral orchitis may develop and impair semen parameters albeit transiently. The long term effects still need to be evaluated.[6]
COVID-19 infection in pregnant women is more severe than their nonpregnant counterparts with increased morbidity and mortality and adverse perinatal outcome in the form of preterm birth, growth restriction, still birth and increased caesarean delivery.[7,8]
Also vertical transmission though not proven is still a possibility.[9]
The psychological effects of stress due to fear of the disease, social restrictions and financial implications may also disturb the HPO axis.
Drugs used in the treatment of COVID-19 infection and sanitization agents in the environment may also result in changes at the molecular level and have a bearing on the fertility potential of a couple.[4]
Most scientific societies have advocated that people of reproductive age whether planning conception or not should receive covid vaccine.[10]
RECOMMENDATION Even though the evidence is scant, it is important to prevent this infection as well as augment immunity against this infection prior to commencing fertility treatment.
IFS therefore recommends vaccination before initiating fertility treatment. However, certain circumstances may warrant initiation of treatment before taking the vaccine, for instance,
scarcity or non-availability of vaccine in some states,
medical conditions like fertility preservation for cancer, advanced age, poor ovarian reserve etc.
In these circumstances, the patient may be advised to initiate treatment but the final decision may be left to the patient after explaining all pros and cons and an informed consent taken before starting treatment. The vaccine can be taken as and when it becomes available.
Prevention of infection
Though risk mitigation measures like wearing a mask, maintaining hand hygiene and social distancing remain the best preventive strategy, availability of vaccines have provided a new hope of curtailing the virus and averting further waves of COVID-19.
So, couples are advised to continue with efforts at conception, follow all preventive measures and meanwhile seek vaccination at the earliest.[11]
Generally, any vaccine which is available can be taken by those seeking pregnancy with the exception of live attenuated one to avoid harm in case of accidental pregnancy.
For patients who have already been infected with COVID, IFS advises to take the vaccination in order to enhance their immunity and dampen the effect of a re infection if it occurs.
The various covid vaccines are being developed using different platforms like nucleic acid based, viral vector based, protein and peptide subunit based, killed whole virus, nanoparticle and virus like particle based vaccines.
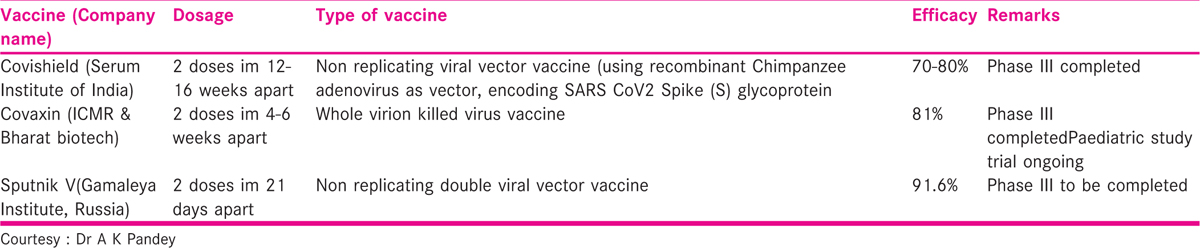
The COVID-19 vaccines approved in our country and the ones in the pipeline are shown in Tables 1 and 2

Other international vaccines which may be available in near future in our country are
mRNA based vaccines- BioNTech/ Pfizer and Moderna. These do not contain the COVID-19 virus and so theoretically cannot lead to infection. In addition, they do not interact with the host’s DNA and so cannot cause genetic changes.
Viral vector vaccine − Jannsen (Johnson & Johnson) single dose vaccine, Oxford- Astrazaneca
Inactivated Virus vaccine: Coronavac, Sinopharm
Protein based- Novavax
Most vaccines have either no or minimal minor side effects like immediate pain, sweating and nausea after receiving the vaccine. There could be fever, fatigue, myalgia, arthralgia, lymphadenopathy, local pain, swelling, redness, rash and diarrhea in the first week after the vaccine. Most of these adverse effects can be alleviated by simple medications.[12] Rarely there may be severe anaphylactic reactions, thromboembolic phenomena resulting in cardiopulmonary or cerebrovascular events, severe gastrointestinal disturbances, facial palsy and local infections like cellulitis.
RECOMMENDATION
IFS strongly recommends all preventive measures including vaccination to mitigate the possibility of infection to all those planning a pregnancy or contemplating ART treatment. Any of the available vaccines in the country may be taken.
There are many queries in the minds of the patients which need to be addressed. However, because of limited knowledge about the disease and the daily emerging evidence, it is recommended that the final decision to vaccinate should be left to the couple or the individual seeking advice.
Similarly, the advice to the person seeking opinion would be that although covid vaccines have been developed in a short time frame, they seem to be safe and efficacious. The final decision to accept or decline the vaccine by couples desiring conception and those who are pregnant should be in consultation with a healthcare professional after understanding the benefits and presumed risks as more evidence continues to evolve.
The present guidance attempts to provide answers to most of the queries raised.
FREQUENTLY ASKED QUESTIONS
Vaccination during pregnancy
The MoHW has recently approved of the use of all vaccinations available in India for use during pregnancy.
A pregnant woman who opts for vaccination, could be vaccinated at any time of the pregnancy. To help pregnant women make an informed decision to be vaccinated, they should be provided with information about the risks of COVID-19 infection in pregnancy, the benefits of vaccination, along with the likely side effects of vaccination. The reader is referred to the MoHW site for detailed information on vaccination in pregnancy (22).
Recommendation
In view of the serious outcomes of COVID during pregnancy in some cases, IFS strongly endorses and recommends the use of vaccines during pregnancy. Patients may take the first dose before or during commencement of ART treatment and follow up the second dose during pregnancy. It is preferred that the second dose be taken at the end of first trimester although it can be taken at any time, in any trimester.
COLLABORATORS
We thank the following chapter secretaries of all IFS chapters for their valuable inputs and help in the preparation of this document. Dr Anju Mathur., Dr Sarabjeet Singh, Dr Sonu Balhara, Dr Shashi Bala, Dr Firuza Parekh, Dr Akshaya Mahapatro, Dr Rajapriya Ayyappan, Dr Himanshu Roy, Dr Anupam Gupta, Dr Ritu Prasad, Dr Syed Hussain, Dr Sushma Deshmukh, Dr Divyashree PS, Dr Yatinder, Dr Sunita Chandra, Dr Veronica Yuel, Dr Venugopal, Dr Papa Dasari, Dr Alok Sharma, Dr Archana, Dr Jayesh Amin, Dr Madhab Das, Dr Nitin Lad, Dr Roza Rozati, Dr Usha, Dr Mujibur Rehman, Dr Rashmi Shirish, Dr Surender Kumar
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We thank Dr AK Pandey MBBS, MD, Dean Academics & Chief Collaborator Molecular Biology Lab ESI Hospital, Faridabad, for his valuable inputs on the vaccines.
REFERENCES
- Genome Composition and Divergence of the Novel Coronavirus (2019 -nCoV) Originating in China. Cell Host Microbe [Internet]. 2020;27(3):325-8. [cited 2021 Jun 7]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7154514/
- [Google Scholar]
- Novel coronavirus: From discovery to clinical diagnostics. Infect Genet Evol. 2020;79:104211.
- [Google Scholar]
- SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271-280.e8.
- [Google Scholar]
- Potential risks of SARS-CoV-2 infection on reproductive health. Reprod Biomed Online [Internet]. 2020;41(1):89-95. [cited 2021 Jun 8]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7192111/
- [Google Scholar]
- Potential effects of COVID-19 on reproductive systems and fertility; assisted reproductive technology guidelines and considerations: a review. Hong Kong Med J [Internet] 2021 Apr 15 [cited 2021 Jun 8]; Available from: https://www.hkmj.org/abstracts/v27n2/118.htm
- [Google Scholar]
- Male Fertility and the COVID-19 Pandemic: Systematic Review of the Literature. World J Mens Health [Internet]. 2020;38(4):506-20. [cited 2021 Jun 8];Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7502312/
- [Google Scholar]
- A comprehensive review of the impact of COVID-19 on human reproductive biology, assisted reproduction care and pregnancy: a Canadian perspective. J Ovarian Res. 2020;13(1):140.
- [Google Scholar]
- Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320.
- [Google Scholar]
- Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224(1):35-53.e3.
- [Google Scholar]
- BFS & ARCS Covid-19 Vaccines & Fertility [Internet]. British Fertility Society | BFS; 2021. [cited 2021 Jun 8]. Available from: https://www.britishfertilitysociety.org.uk/2021/02/09/bfs-arcs-covid-19-vaccines-fertility/
- Joint IFFS/ESHRE statement on COVID-19 vaccination for pregnant women and those considering pregnancy. Hum Reprod Open. 2021;2021(2):hoab016.
- [Google Scholar]
- Does mRNA SARS-CoV-2 vaccine influence patients’ performance during IVF-ET cycle? Reprod Biol Endocrinol. 2021;19(1):69.
- [Google Scholar]
- Covid-19: No evidence that vaccines can affect fertility, says new guidance. BMJ. 2021;372:n509.
- [Google Scholar]
- Coronavirus disease2019 vaccine response in pregnant and lactating women: a cohort study. American Journal of Obstetrics & Gynecology [Internet] 2021 Mar 25 [cited 2021 Jun 8];0(0). Available from: https://www.ajog.org/article/S0002-9378(21)00187-3/abstract
- [Google Scholar]
- Vaccinating Pregnant and Lactating Patients Against COVID-19 [Internet]. [cited2021 Jun 8]. Available from: https://www.acog.org/en/clinical/clinical-guidance/practice-advisory/articles/2020/12/vaccinating-pregnant-and-lactating-patients-against-covid-19
- American Society for Reproductive Medicine (ASRM) Position on COVID Vaccine Use in Pregnant Women [Internet]. [cited2021 Jun 8]. Available from: https://www.asrm.org/news-and-publications/news-and-research/press-releases-and-bulletins/american-society-for-reproductive-medicine-asrm-position-on-covid-vaccine-use-in-pregnant-women/
- SMFM_Vaccine_Statement_12-1-20_ (final).pdf [Internet]. [cited2021 Jun 8]. Available from: https://s3.amazonaws.com/cdn.smfm.org/media/2591/SMFM_Vaccine_Statement_12-1-20_(final).pdf
- Coronavirus Disease 2019 (COVID-19) Vaccines and Pregnancy. Obstet Gynecol [Internet]. 2021;137(3):408-14. [cited 2021 Jun 8]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7884084/
- [Google Scholar]
- COVID-19 vaccines, pregnancy and breastfeeding [Internet] Royal College of Obstetricians & Gynaecologists. [cited 2021 Jun 8]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/coronavirus-covid-19-pregnancy-and-womens-health/covid-19-vaccines-and-pregnancy/covid-19-vaccines-pregnancy-and-breastfeeding/
- [Google Scholar]
- Joint Statement Regarding COVID-19 Vaccine in Men Desiring Fertility from the Society for Male Reproduction and Urology (SMRU) and the Society for the Study of Male Reproduction (SSMR) [Internet]. [cited2021 Jun 8]. Available from: https://www.asrm.org/news-and-publications/covid-19/statements/joint-statement-regarding-covid-19-vaccine-in-men-desiring-fertility-from-the-society-for-male-reproduction-and-urology-smru-and-the-society-for-the-study-of-male-reproduction-ssmr/








